
CLAIMS.AI is an AI-powered solution that automates claims management, predicting and preventing denials to improve accuracy and boost payer reimbursements for healthcare providers.
Vendor
BUDDI AI
Company Website
CLAIMS.AI is a sophisticated claim denial prediction and prevention engine designed to revolutionize claims management for healthcare providers. Leveraging deep-learning technology, the platform automates the complex process of claims submission and reconciliation, leading to more accurate claims, a significant reduction in denials, and ultimately, higher payer reimbursements. It meticulously analyzes a vast array of historical data, including past denials and approvals, Explanation of Benefits (EOBs), medical codes, CARC/RAC codes, and payer payment patterns. This comprehensive analysis allows CLAIMS.AI to proactively identify potential errors and issues before a claim is even submitted, drastically decreasing the odds of denial. Clients who have implemented CLAIMS.AI have reported an impressive average reduction of 40% in claim denials within just 12 months of deployment. This reduction directly translates into substantial financial benefits. Given that a typical health system can lose as much as 3.3% of net patient revenue due to denials, CLAIMS.AI empowers providers to capture previously lost revenue, significantly improving their bottom line and operational efficiency by transforming claims into a more predictable and profitable process.
Features & Benefits
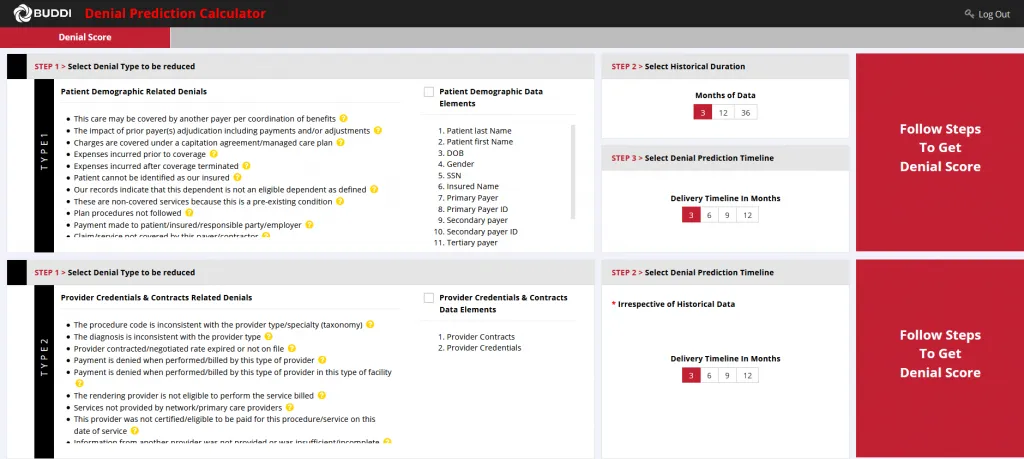
- Claim Denial Prediction and Prevention Engine
- Leverages deep-learning to automate claims management, resulting in more accurate claims, significantly reduced denials, and higher payer reimbursements.
- Improved Claims Accuracy
- Analyzes historical denials and approvals, EOBs, medical codes, CARC/RAC codes, payment patterns, and other payer behavior to proactively identify errors before claim submission, decreasing odds of denial.
- Reduced Claim Denials
- Clients deploying CLAIMS.AI report an average 40% reduction of denials within 12 months of launch.
- Boosted Payer Reimbursements
- By significantly reducing denials, providers can capture more revenue and improve their bottom line, addressing potential losses of up to 3.3% of net patient revenue.